Table of Contents
- Background
- Case Studies
- Product Catalog
Background
For cancer patients, the world of treatments is rapidly changing and growing, offering cutting-edge technology, and promising new methods of fighting the disease. But as all journeys must begin with a first step, so does the path to recovery in cancer treatment, and this first step traditionally involves hematoxylin and eosin (H&E) staining. Intraoperative frozen-section consultation is one such avenue of H&E frequently used, where slides are prepared from frozen tissue mass. H&E staining is a rapid enough process to generate results usually within 30-60 minutes.
This method has issues however, particularly with the freezing process damaging tissue morphology, making the results difficult to interpret. Unfortunately, oftentimes these difficulties lead to misdiagnosis, necessitating further testing or even repeating surgery for the patient – a process that is taxing in time, money, and mental stress for all involved.
Immunohistochemistry (IHC) staining offers a solution to this by increasing operator confidence compared to H&E staining, since IHC staining shows biomarker expression in addition to the general morphology of the tissue. The drawback to this historically, however, is that the process can be very time-consuming and can take hours to complete. With that turnaround rate, IHC is not used during the intraoperative phase despite its advantages, restricted to post-operational diagnostics, where it can take 1-2 days to process and interpret. During this time, surgeons may need to decide on how to proceed without having complete certainty in what they’re dealing with.
But what if speed was no longer a factor? Celnovte Biotechnology’s PolyStackerTM detection technology guarantees results within the acceptable timeframe with a turnaround time as short as 10-15 minutes to assist in diagnosing cancer – all intraoperatively. This rapid IHC protocol is used in parallel with H&E staining to give a full picture of the nature of the tissues sample, assisting surgeons in making decisions for next steps.
The technology promises rapid detection of tumor markers, reduced false negative rates, increased accuracy in diagnosing challenging cases (metastatic microlesions, infiltrative microlesions) and comparable match rates to post-operative traditional FFPE IHC results. With this, surgical decisions can be made with increased confidence and less stress for patients and surgeons alike, allowing for more informed decision making when choosing the next steps in treatment and can save precious time in the fight against cancer.
Case Studies
The efficacy of Celnovte Biotechnology’s frozen section rapid IHC technology can be observed in the following case study. In this example, doctors in China cite an example of lung cancer where rapid IHC was used. The patient, a 67-year-old female, was admitted to the hospital and underwent surgical treatment due to nodules seen in a CT scan that were not responsive to anti-inflammatory treatment.
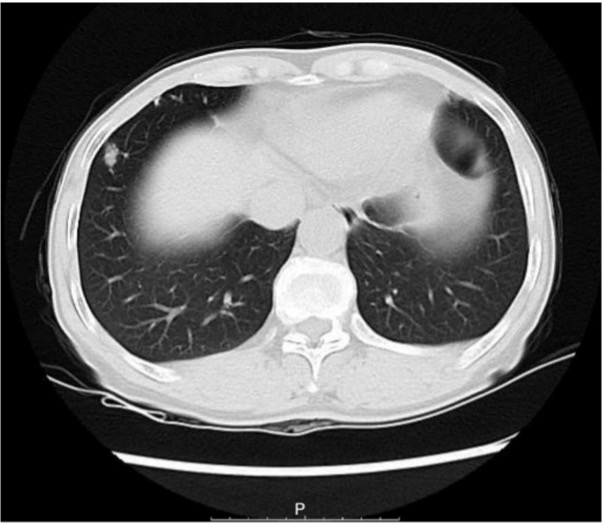
Figure 1 – CT scan of patient in case study 1, the bilateral thorax was symmetrical, and no obvious abnormalities were found. The trachea is centered, and the tracheobronchial tree is unobstructed. A solid nodule (thin layer lm373) was found in the lower lobe of the right lung, with a long diameter of approximately 11.3 mm. There are a few micronodules in both lungs. The structure of the bilateral lung hilum was clear, and there were no obvious abnormalities in shape, size, and position. There was no abnormal enlargement of lymph nodes in each group of mediastina.
Frozen section diagnosis was used to determine the nature of the nodules to determine malignancy of the observed growths. The patient underwent partial lung tissue resection of the right lower lobe which was sent for freezing and used in both H&E as well as rapid IHC tissue testing.
For H&E, many lymphocyte cells were seen, however no obvious malignant lesions were found.
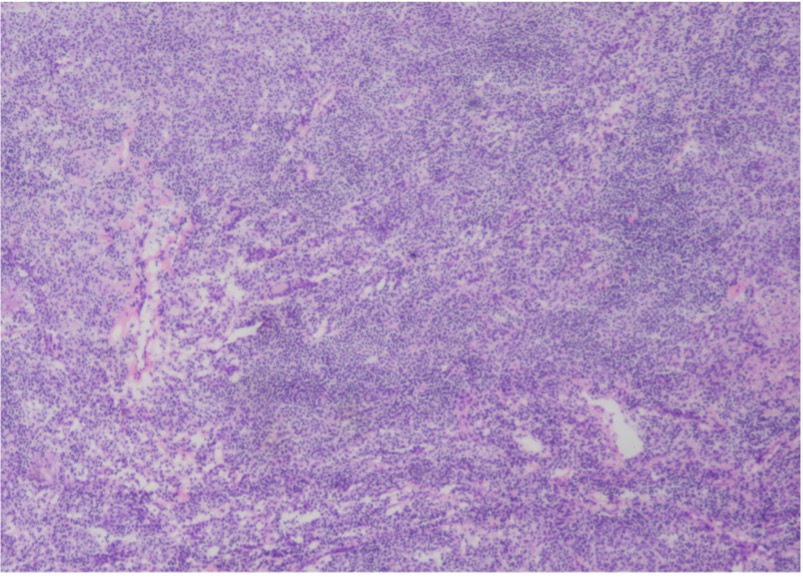
Figure 2 – H&E staining of tissue section from lower right lung, 120x40x15mm in size. Lymphoid tissue proliferation was seen in the sections, and no obvious malignant lesions were found under routine H&E staining.
Due to the application of rapid IHC for the frozen section, it can be observed that small focal clusters of epithelial cells were seen in the sections via CK staining, which was considered an epithelial malignant tumor.
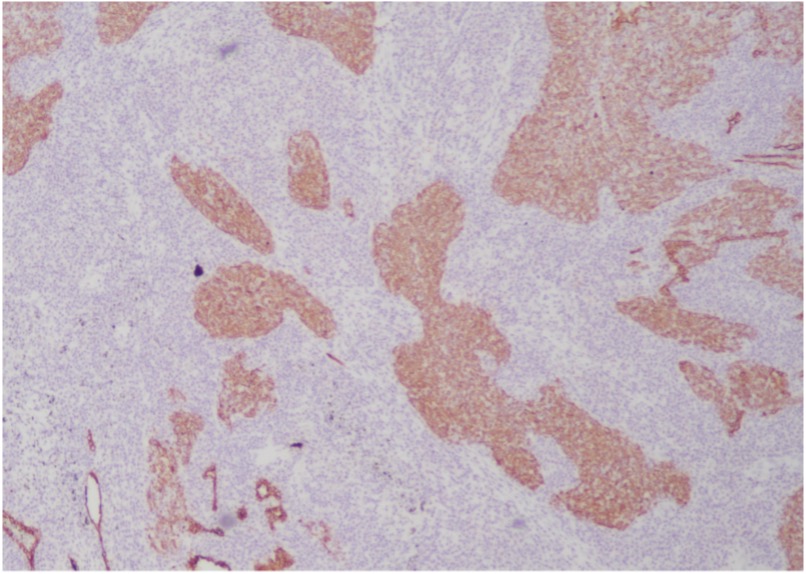
Figure 3 –Celnovte Biotechnology frozen section rapid IHC staining of tissue section from lower right lung, 120x40x15mm in size. After CK staining, small focal clusters of epithelial cells were seen in the sections, which was considered an epithelial malignant tumor.
In conjunction with the H&E staining results, surgeons were able to intraoperatively move forward with the working assumption that the tissues were positive for lymphoepithelial carcinoma, an assumption they would’ve been unable to make in the operating room if they had only used H&E staining. Further FFPE IHC testing with CK, P40 and in situ hybridization EBER and a noted absence of nasopharyngeal tumors confirmed the assumption and diagnosed the patient with lymphoepithelial carcinoma.
In this case, Celnovte Biotechnology’s frozen section rapid IHC was used to show the presence of difficult to see lymphoepithelial carcinoma cells. Due to the large volume of lymphocytes in the selection, it would be especially difficult to see these squamous/undifferentiated cells as they can be overshadowed with so few and small cell clusters. Because of the use of rapid IHC, the diagnosis was correctly made where it would otherwise be easy to misdiagnose these tumor cells despite them being in the early stages of growth where lesions are less obvious.
Product Catalog
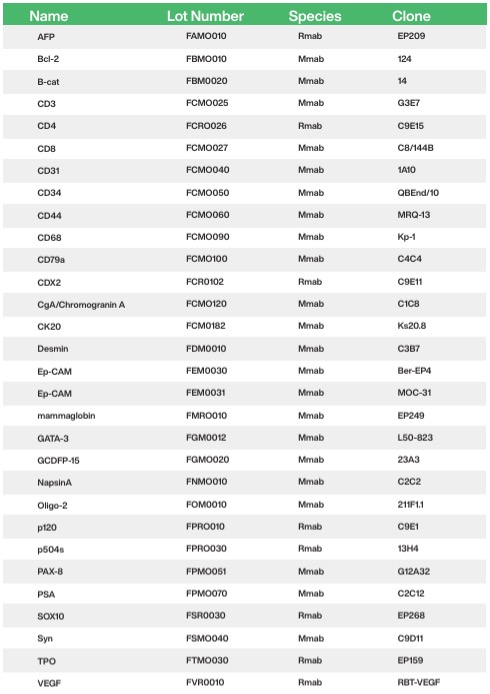
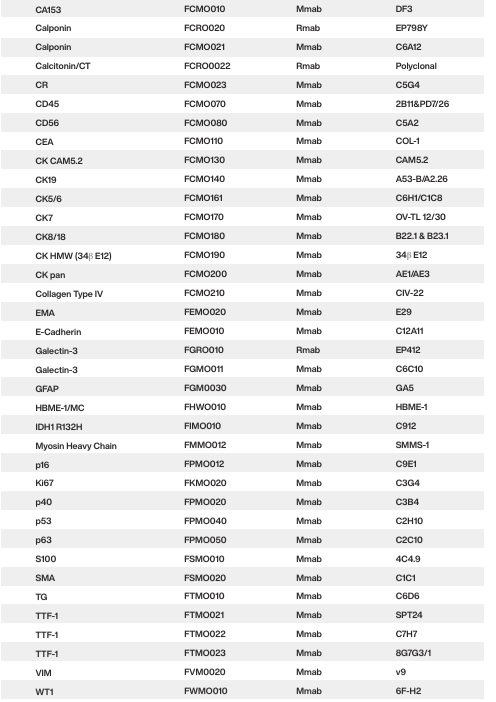
📣 Contact us now
Celnovte is a rapidly expanding global company, and we invite you to join us in growing our businesses together. ☺️ Contact us now
Case Study丨Application of CELNOVTE Intraoperative Rapid Immunohistochemistry in the Diagnosis of Bronchiolar Adenoma and Lung Adenocarcinoma
Patients with pulmonary bronchiolar adenoma (BA) usually have no obvious clinical symptoms, and almost all diagnoses are first discovered via CT scan images. However, since BA imaging manifestations are difficult to differentiate from early malignant tumors, intraoperative frozen section pathology diagnosis is a necessary step [1].
Because the peripheral lung tissue of proximal BA is often rich in mucus cells, it needs to be distinguished from invasive mucinous adenocarcinoma. Distal BA luminal cells lack mucin and ciliated cells, or even only Clara or alveolar cells, so they are easily confused with non-mucinous adenocarcinoma in situ, minimally invasive adenocarcinoma, or even invasive adenocarcinoma. Due to the unclear cell ciliary structure on frozen sections, the interstitium is widened and it is difficult to determine whether there are basal cells, which can easily be confused with invasive mucinous adenocarcinoma and well-differentiated acinar adenocarcinoma, leading to misdiagnosis [2-3].
Immunohistochemistry to determine the presence of continuous basal cells is an important basis for diagnosis. Intraoperative rapid immunohistochemistry for CK5/6 and other antibodies can assist in differential diagnosis.
Clinical information:
The patient was a 65-year-old female. The frozen section (nodule in the lower lobe of the left lung) showed a gray-white nodule with a diameter of 1 cm.
01 Intraoperative H&E staining:

For lesions with a clear boundary around the bronchus in lung tissue, columnar/cuboidal epithelium can be seen growing in adenoid, papillary or adherent form, and it is necessary to differentiate between invasive carcinoma and bronchiolar adenoma.
02 Intraoperative rapid immunohistochemistry

Intraoperative rapid immunohistochemistry on frozen sections for CK5/6 (-) showed no basal cells, consistent with invasive adenocarcinoma.
03 Postoperative H&E staining

The postoperative paraffin H&E staining results were consistent with the intraoperative staining results.
04 Postoperative immunohistochemistry
Paraffin section immunohistochemistry for p40-, TTF-1+, Napsin A(+).
p40 negative

TTF-1 positive

Napsin A positive

Diagnostic result:
The final diagnosis based on histomorphology and immunohistochemistry: invasive adenocarcinoma, non-mucinous type, moderately differentiated.
Further Content – Statistics Based Evidence for the Efficacy of Interoperative Rapid IHC
At present, intraoperative frozen section H&E staining technology is an important means to quickly determine the nature of specimen lesions during surgery and guide the surgical method and scope. However, the morphology of tissue cells in some diseases is relatively similar, making it difficult to identify by H&E staining alone. It is easy to miss or misdiagnose, and even cause Patient’s secondary surgery or medical accident.
Han, Liyuan et al.[4] conducted a comparative analysis of the pathological diagnosis results of intraoperative frozen sections and postoperative paraffin sections and immunohistochemistry pathology diagnosis results. They found that the accuracy of intraoperative frozen section pathological examination in differential diagnosis of benign and malignant pulmonary nodules was 99.2. %, and the accuracy of classifying lung malignant tumors was 85.3%.
Shen, Yuanlong et al. [5] used paraffin section immunohistochemistry confirmed pulmonary sclerosing pneumonitis (PSP) and lung adenocarcinoma tissues as the research subjects. By comparing the TTF-1, ER and Ki-67 expression, it was found that the diagnosis accuracy of intraoperative rapid immunohistochemistry and intraoperative H&E staining for PSP were 100.00% and 58.33% respectively, and the accuracy for diagnosing lung adenocarcinoma were 96.15% and 76.92% respectively (Table 1). This indicates that rapid intraoperative frozen section immunohistochemistry can significantly improve the accuracy of diagnosis of PSP and lung adenocarcinoma. Furthermore, by comparing the differential expression results of TTF-1, ER and Ki-67 in the two diseases, it was found that they can be used as indicators of rapid intraoperative frozen section immunohistochemistry for differential diagnosis of the two diseases.
Table 1 – Comparison of the accuracy of intraoperative frozen section rapid immunohistochemistry and H&E staining in the diagnosis of PSP and lung adenocarcinoma

Note: * P<0.05, Fisher’s exact test
In addition, a comparison of the rapid immunohistochemical staining results of intraoperative frozen sections and the immunohistochemical staining results of paraffin sections showed that there was no significant difference between the two. This confirms that rapid immunohistochemical staining of intraoperative frozen sections has practical clinical significance for the differential diagnosis of PSP and lung adenocarcinoma.
Intraoperative frozen section rapid immunohistochemistry is performed simultaneously with intraoperative frozen section H&E staining. A report is issued within 30 minutes after the specimen is received in the pathology department, which does not affect the reporting time of frozen diagnosis. At the same time, not only can intraoperative rapid frozen section immunohistochemistry improves the accuracy of diagnosis, it can also significantly shorten the patient’s pathological waiting time and provide a reliable basis for adjusting the surgical plan.
References:
[1] WANG Yingxia; TIAN Yang; ZHAO Wen; ZHANG Xuan. Clinicopathological analysis of 24 cases of bronchiolar adenoma. Journal of Clinical and Pathological Research. 2023,43(05):880-887. (in Chinese)
[2] Liu S, Liu N, Xiao M, Wang L, Wang EH. First case of bronchiolar adenoma lined purely by mucinous luminal cells with molecular analysis: A case report. Medicine (Baltimore). 2020 Sep 25;99(39):e22322.
[3] ZHU Hao-hao; REN Guang-yu; WEN Jian-feng. Several benign pulmonary diseases easily misdiagnosed during intraoperative frozen sections. Chinese Journal of Diagnostic Pathology. 2023,30(07):701-703, 707. (in Chinese)
[4] HAN Liyuan; CUI Yayan; CHEN Dong; MEI Shaoshuai; LIAN Guoliang. Study on pathological diagnosis of pulmonary nodules in frozen operation. Journal of Cardiovascular and Pulmonary Diseases. 2022,41(03):302-305, 308. (in Chinese)
[5] SHEN Yuanlong; LI Lin; WU Zihao. Comparison of the application of intraoperative frozen section rapid immunohistochemistry and HE staining in the diagnosis of sclerosing pneumoma and lung adenocarcinoma. Anhui Medical Journal. 2019,40(12):1392-1395. (in Chinese)